Back to the Basics – Airway Anatomy, Part 1

How often do you think about breathing? Probably not too often—unless you find yourself struggling to breathe. When that happens, breathing becomes all you can focus on.
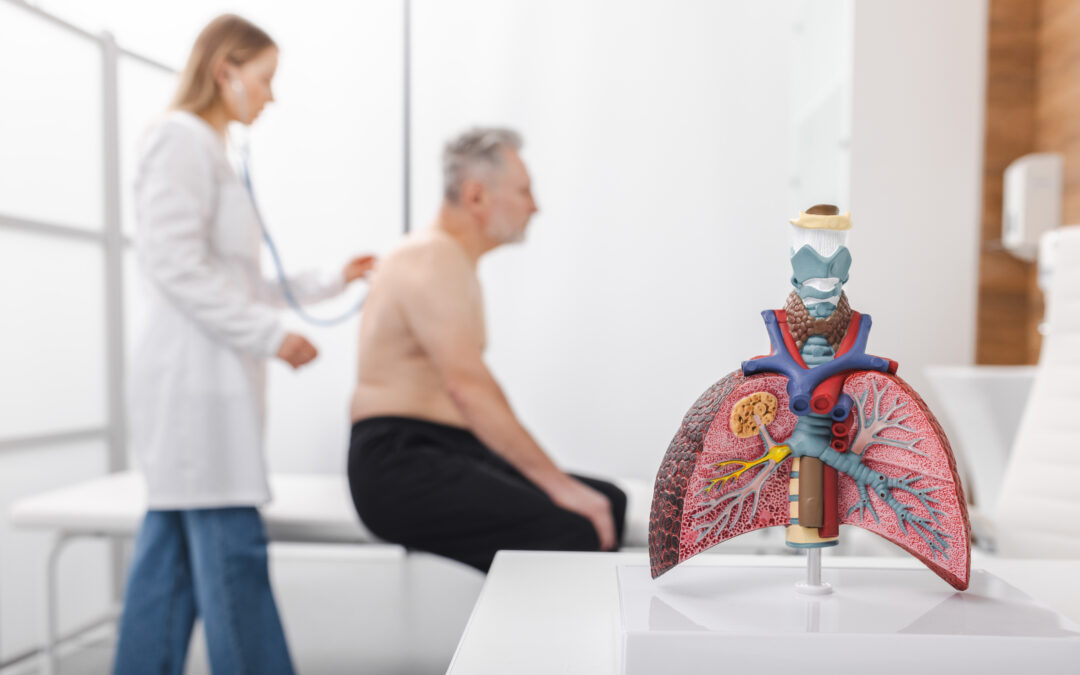
The pulmonary, or respiratory, system is complex. Organs and tissues work together to allow us to breathe and exchange gases within the body. The primary function of the respiratory system is to draw in oxygen and expel carbon dioxide. This gas exchange helps maintain the body’s homeostasis, including acid–base balance and blood pH. The lungs, which are the major organs of the respiratory system, exchange gases across approximately 70 square meters of epithelial surface area. For perspective, this is roughly one‑fourth the size of a tennis court.
The respiratory system is divided into two parts: the upper respiratory tract and the lower respiratory tract, also referred to as the extrathoracic and intrathoracic airways. Breathing is regulated by the autonomic nervous system (ANS), which controls unconscious processes in the body, including respiration. The ANS connects the brain to most internal organs, including those of the respiratory system.
Anatomy of the Upper Airway
The upper airway includes the nose, mouth, and larynx. The larynx serves as the anatomical border between the upper and lower airways.
The upper airway functions as a conduit for gases traveling to and from the lungs and serves as the respiratory system’s first line of defense. In patients with airway disease, symptoms may originate in or involve both the upper and lower airways, making assessment of both regions essential.
The Nose
The nose is a complex structure responsible for warming, humidifying, and filtering inhaled air. This is accomplished through three pairs of turbinates, or conchae—folds of tissue that warm and moisturize air, bringing it close to body temperature even in dry conditions. The nose also filters debris from inhaled air. Cilia, small hair‑like structures lining the nasal passages, trap dirt and particles before they enter the lower airway.
Air flows in and out through two nasal cavities, which are lined with mucous membranes. The paranasal sinuses are air‑filled spaces that produce mucus to keep the nasal passages moist.
When assessing a patient for asthma, evaluation of the nose is an important but sometimes overlooked step. Does the patient have concurrent rhinosinusitis? Are nasal polyps present? Nasal polyps—soft, painless, noncancerous growths—are commonly seen in patients with asthma and can obstruct nasal airflow. Chronic rhinosinusitis is a prevalent condition, affecting up to 12% of adults. While not all patients with chronic rhinosinusitis have nasal polyps, chronic rhinosinusitis with nasal polyps (CRSwNP) is associated with Type 2 inflammation, which is also linked to asthma and other inflammatory diseases. Up to 19% of patients with severe asthma have comorbid CRSwNP.
The Pharynx and Larynx
Continuing through the upper airway, the pharynx (throat) is divided into three regions: the nasopharynx, oropharynx, and laryngopharynx. The nasopharynx is located at the back of the nasal cavity and functions as a passageway for air. The oropharynx lies at the back of the mouth and contains the tonsils. The laryngopharynx connects the larynx to the esophagus.
The larynx is composed of nine cartilages. One of these, the epiglottis, acts as a protective valve, closing during swallowing to prevent aspiration of food into the trachea. During breathing and speech, the epiglottis remains open, allowing air to pass through. The larynx also contains the vocal folds, which vibrate to produce sound.
When evaluating a patient for asthma, it is essential to determine whether reported symptoms are truly due to asthma or caused by a common asthma mimic, vocal cord dysfunction (VCD). VCD can sound and present like asthma, and patients may have both conditions simultaneously. Because treatment strategies differ significantly, accurate identification of one or both conditions is critical.
In a retrospective study of 292 patients with VCD, asthma, coexisting VCD and asthma, and control subjects, asthma and VCD coexisted in 32.6% of patients with VCD. Additionally, 42% of patients with VCD had been misdiagnosed and treated for asthma for up to nine years. These misdiagnosed patients experienced higher healthcare utilization, increased medication use, more emergency department visits, mislabeled asthma exacerbations, and a trend toward increased hospitalizations.
Returning to the basics of airway anatomy and incorporating readily available objective tests—such as spirometry, fractional exhaled nitric oxide (FeNO) measurement, and airway challenge testing, including the methacholine challenge—helps ensure an accurate diagnosis. Objective testing can save patients time, reduce unnecessary costs, and prevent emotional distress by guiding appropriate and effective management.
Author:
Heather Murgatroyd, BA, RRT, CPFT, AE-C
Senior Clinical Specialist
Methapharm Respiratory
References
Lung Anatomy: Overview, Gross Anatomy, Microscopic Anatomy
Medscape.
https://emedicine.medscape.com/article/1884995-overview
22.2 The Lungs – Anatomy and Physiology 2e
OpenStax.
https://openstax.org/books/anatomy-and-physiology-2e/pages/22-2-the-lungs
Basic Airway Anatomy Guide
MedicTests.
https://medictests.com/units/basic-airway-anatomy
Life with Nasal Polyps: The Patient Experience and Opportunities to Improve Care in the U.S. (April 2024)
Asthma and Allergy Foundation of America (AAFA).
https://aafa.org/wp-content/uploads/2024/04/life-with-nasal-polyps-report.pdf
Upper Respiratory System | Respiratory Anatomy
Visible Body.
https://www.visiblebody.com/learn/respiratory/upper-respiratory-system
Proportion of Patients with Severe Asthma and Comorbid Chronic Rhinosinusitis with Nasal Polyps: A Literature Review
Annals of Allergy, Asthma & Immunology, 2024.
https://www.annallergy.org/article/S1081-1206(24)00722-1/abstract
A Retrospective Analysis Comparing Subjects with Isolated and Coexistent Vocal Cord Dysfunction and Asthma
Allergy and Asthma Proceedings, 2013.
https://www.jacionline.org/article/S0091-6749(12)02890-4/fulltext