Understanding Methacholine Chloride

For most Respiratory Therapists, and other health care workers in pulmonary diagnostics, methacholine chloride is a common, well-known bronchoprovocation agent. Provocholine® is the only FDA cleared methacholine chloride available for the methacholine challenge test (MCT). The indication for a methacholine challenge is for the diagnosis of bronchial airway hyperreactivity in adults and pediatric patients five years of age and older who do not have clinically apparent asthma.1 Generally, the first objective test for diagnosing asthma is Spirometry with pre/post bronchodilator challenge. Bronchodilator responsiveness testing determines the degree of improvement of airflow in response to bronchodilator administration as measured by changes in Forced Expiratory Volume in 1 Second (FEV1) and Forced Vital Capacity (FVC).2 Of note, the 2019 Spirometry update distinguishes “bronchodilator responsiveness testing” from “reversibility testing.” The explanation in the update for this verbiage is to avoid inferring that reversibility suggests a complete elimination of airway obstruction.2 When Spirometry does not show bronchodilator responsiveness, >10% of predicted value in FEV1 or FVC7, incorporating a bronchial challenge test (BCT) is an appropriate next step. As stated in the 2017 ERS/ATS technical standards for methacholine challenge testing, if symptoms, spirometry or response to therapy are atypical, a BCT is appropriate and can increase or decrease the probability of asthma.3
What is methacholine chloride? It is a parasympathomimetic (cholinergic) agonist, a synthetic derivative of acetylcholine. To further break this down:
- Parasympathomimetic – this type of drug mimics the effects of acetylcholine on the parasympathetic nervous system (PNS). This type of drug may also be called a cholinergic receptor stimulating agent.
- Parasympathetic nervous system – this is the “rest and digest” system in the human body. It works without conscious effort.4
- Cholinergic – substance that can produce, alter, or mimic the action of acetylcholine
- Acetylcholine – a neurotransmitter which has function in the central and peripheral nervous systems, including involuntary muscle movement. It influences smooth muscle contraction, among other involuntary responses.5
- Agonist – a drug which activates receptors, mimics the action of endogenous (originates within the body) compounds.6
Thus, methacholine chloride agonizes the muscarinic receptors of the bronchial smooth muscles and can eventually cause bronchoconstriction.1
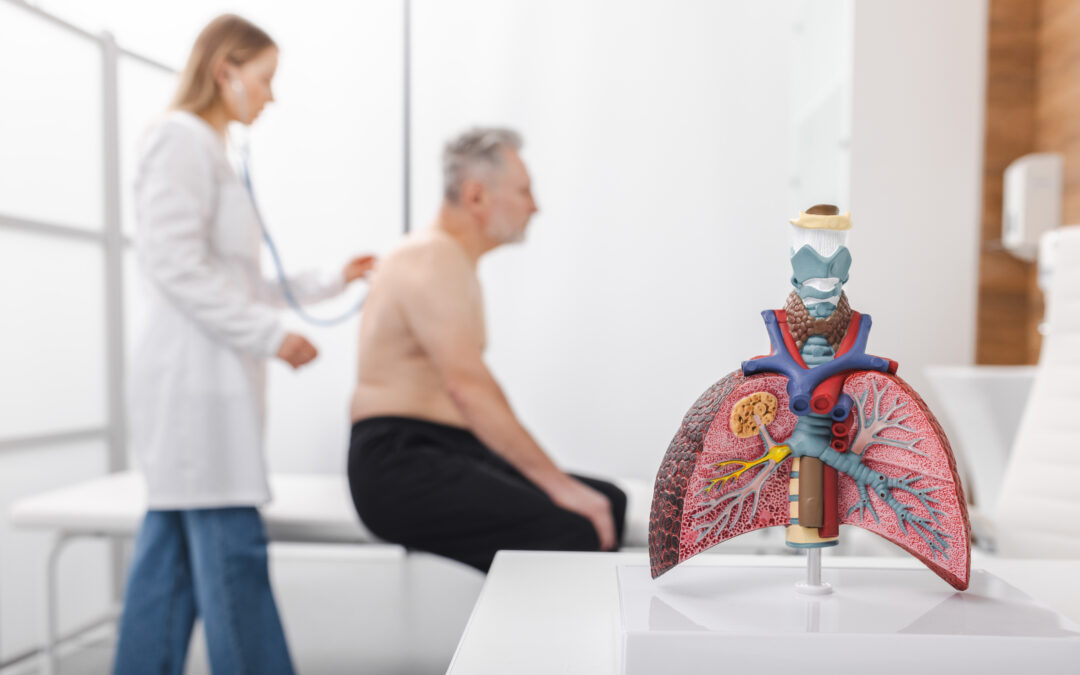
How does methacholine chloride act in the lungs? Bronchial smooth muscles have parasympathetic innervation, people with asthma, or airway hyperresponsiveness, are more sensitive to bronchoconstriction after inhalation of Provocholine® than people without asthma or airway hyperresponsiveness. The strength of the methacholine challenge is in ruling asthma out. The direct challenge tests, as the MCT is categorized, are considered to have high sensitivity, making a negative test helpful in determining current asthma unlikely. When an MCT is positive, unless at a very low dose, the outcome cannot be used to solely to confirm asthma.
Methacholine is metabolized by acetylcholinesterase, which returns nerve cells and their targets to rest after they are activated. It breaks down acetylcholine and disrupts the communication between the nerve cells and target, decreasing acetylcholine’s effectiveness. When acetylcholine molecules reach muscle cells, it binds to cholinergic receptors and eventually cause bronchoconstriction. In the event of a positive MCT or the advent of severe bronchoconstriction, administration of a rapid-acting inhaled B-agonist will expedite the return of the patient’s FEV1 to baseline, within 10 to 20 minutes post administration of B-agonist.1
Bronchial challenge tests are a piece of the puzzle when diagnosing asthma. Along with clinical symptoms and evaluation, Spirometry and evaluating inflammation, bronchial challenge tests complete the patient picture given there is no single “gold standard’ test to diagnose asthma.
For additional information on testing procedure, contraindications and safety please review the Provocholine product insert found at https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e8983096-65e6-41f2-8b6f-bbf0a7227307
Alternatively, for any medical information inquiries regarding Provocholine, you may also reach out to us at medinfo@methapharm.com
Heather Murgatroyd, BA, RRT, CPFT, AE-C
Senior Clinical Specialist
Methapharm Respiratory
2. Standardization of Spirometry 2019 Update An Official American Thoracic Society and European Respiratory Society Technical Statement Brian L. Graham, Irene Steenbruggen, Martin R. Miller, Igor Z. Barjaktarevic, Brendan G. Cooper, Graham L. Hall, Teal S. Hallstrand, David A. Kaminsky, Kevin McCarthy, Meredith C. McCormack, Cristine E. Oropez, Margaret Rosenfeld, Sanja Stanojevic, Maureen P. Swanney† , and Bruce R. Thompson; on behalf of the American Thoracic Society and the European Respiratory Society
3. Coates AL, Wanger J, Cockcroft DW, et al. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J 2017; 49: 1601526 [https://doi.org/10.1183/13993003.01526-2016].
4. What Does The Parasympathetic Nervous System Do?
5. Acetylcholine | Definition, Function, & Facts | Britannica
6. Agonists and Antagonists: Definition, Mechanism and Types – Pharmaacademias
7. Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J 2022; 60: 2101499 [DOI: 10.1183/ 13993003.01499-2021].