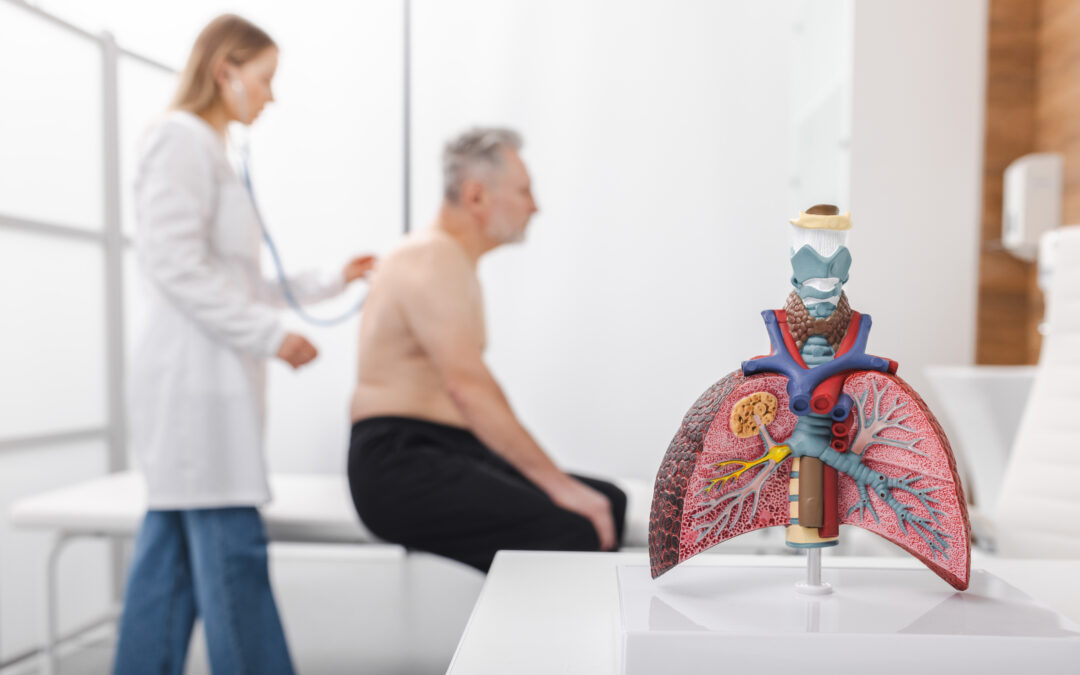
How often do you think about breathing? Probably not too often—unless you find yourself struggling to breathe. When that happens, breathing becomes all you can focus on. The pulmonary, or respiratory, system is complex. Organs and tissues work together to allow us to...