COPD & Emphysema

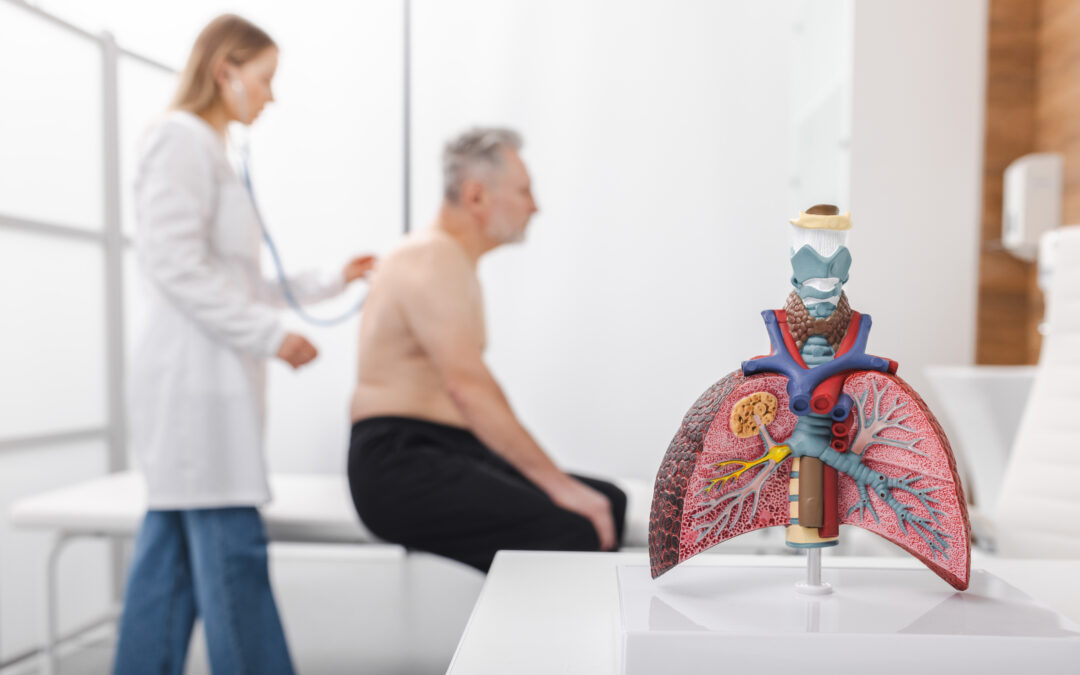
Emphysema is a chronic progressive disease of the airways, specifically the alveoli. Emphysema is the destruction and enlargement of the alveoli. The alveoli are the air sacks located at the ends of the bronchioles (alveolus is the singular or one air sac). The number of alveoli increases rapidly during our first two years of life, increasing more slowly through adolescence. The health of our alveoli is essential as this is where gas exchange occurs. The surrounding capillaries transport oxygen into the body and facilitate the removal of the waste product carbon dioxide. Inflammation and chronic oxidative stress are contributing factors in the damage to the alveoli. Emphysema is part of the structural changes seen in some patients with chronic obstructive pulmonary disease (COPD). COPD was first identified over 200 years ago and is now one of the three top causes of death worldwide. Approximately three million deaths globally are attributed to COPD annually, and approximately 3 million people in the USA have emphysema. Emphysema is most often caused by smoking or exposure to toxic particles from household or outdoor air pollution.
Interestingly, only a small number of smokers develop significant emphysema, so genetic factors may also play a role. There is a genetic, familial form of emphysema, Alpha 1 Antitryspin Deficiency Syndrome. As with other pulmonary diseases, COPD and emphysema require objective testing along with evaluation of symptoms for proper diagnosis. Commonly reported symptoms include dyspnea, wheezing, chest tightness, fatigue, cough with or without sputum production, and activity limitations. Many symptoms are shared with other pulmonary diseases, non-pulmonary diseases, and even acute illnesses, making objective testing an essential component of the diagnostic process.
The symptoms of emphysema develop slowly over time. Smoking-related emphysema symptoms typically begin between 40-60 years of age. The main symptoms are shortness of breath (SOB) with activity and, eventually, SOB at rest as well. Additional emphysema symptoms include cough, phlegm production, wheezing, muscle, and weight loss. Objective tests for diagnosing and identifying COPD and emphysema include pulmonary function testing, chest x-ray, CT scan, arterial blood gas, pulse oximetry and electrocardiogram. How are the objective tests useful for determining emphysema? Emphysema reduces the elastic recoil of the lung parenchyma (tissue) which affects the ability of the lungs to remain open during exhalation, contributing to difficulty in emptying the lungs. The destruction of the parenchyma and additional airway abnormalities leads to hyperinflation at rest and/or with activities. We can see this during pulmonary function testing, specifically in lung volume testing. The effects of emphysema can also be seen in decreasing DLCO (diffusing lung capacity) as we measure gas exchange. Emphysema, which is considered a hallmark of COPD, can be identified and quantified through lung imaging. A lung CT scan can be helpful when considering treatment for emphysema, such as endobronchial valve therapy for a patient. Pulse oximetry or arterial blood gases can determine if a patient needs and qualifies for oxygen therapy.
While emphysema cannot be cured, symptoms and progression can be managed to enhance the quality of life for patients. Smoking cessation must be encouraged. Counseling from physicians and other health professionals, along with nicotine replacement therapy and medications, are shown to increase success in long-term cessation. Education on certain drugs, how to properly use inhaled medications, pulmonary rehabilitation, exercise, staying up to date on vaccinations, and minimizing exposure to indoor and outdoor pollution all contribute to successful management to avoid exacerbations. Patients should be encouraged to participate in the decision- making and management of their chronic disease. For example, do they feel their inhaled medications are working? Are they able to physically initiate the device to receive the medication properly? Are they able to coordinate their breathing with the dispensing of the medication? Can they afford the prescribed medication? As a patient’s disease progresses, they may need to be evaluated for supplemental oxygen or non-invasive positive pressure ventilation (NPPV). Establishing open communication with patients early in the disease process may help to ease the addition of more complex therapies like NPPV.
Encouraging the patient to take an active role in managing their disease daily is essential. Physicians, Respiratory Therapists, and Nurses can provide education and supportive coaching through one-to-one counseling or in group settings. Comprehensive education provides the information patients need to make healthy decisions regarding behavior changes and develop skills to manage their disease. Support from the health care team sets the patient up for self-management. Empowering patients to self-manage has been shown to increase quality of life and reduce respiratory – related hospitalizations. Self-management does not eliminate the need for regular check – ups or evaluations by health care professionals; rather it motivates and increases patient confidence through the continuing support of their health care team.
References
2024 GOLD Report – Global Initiative for Chronic Obstructive Lung Disease – GOLD
Emphysema | American Lung Association
Author: Heather Murgatroyd, BA, RRT, CPFT
Senior Clinical Specialist