The Four Pillars of Asthma Diagnosis and Management

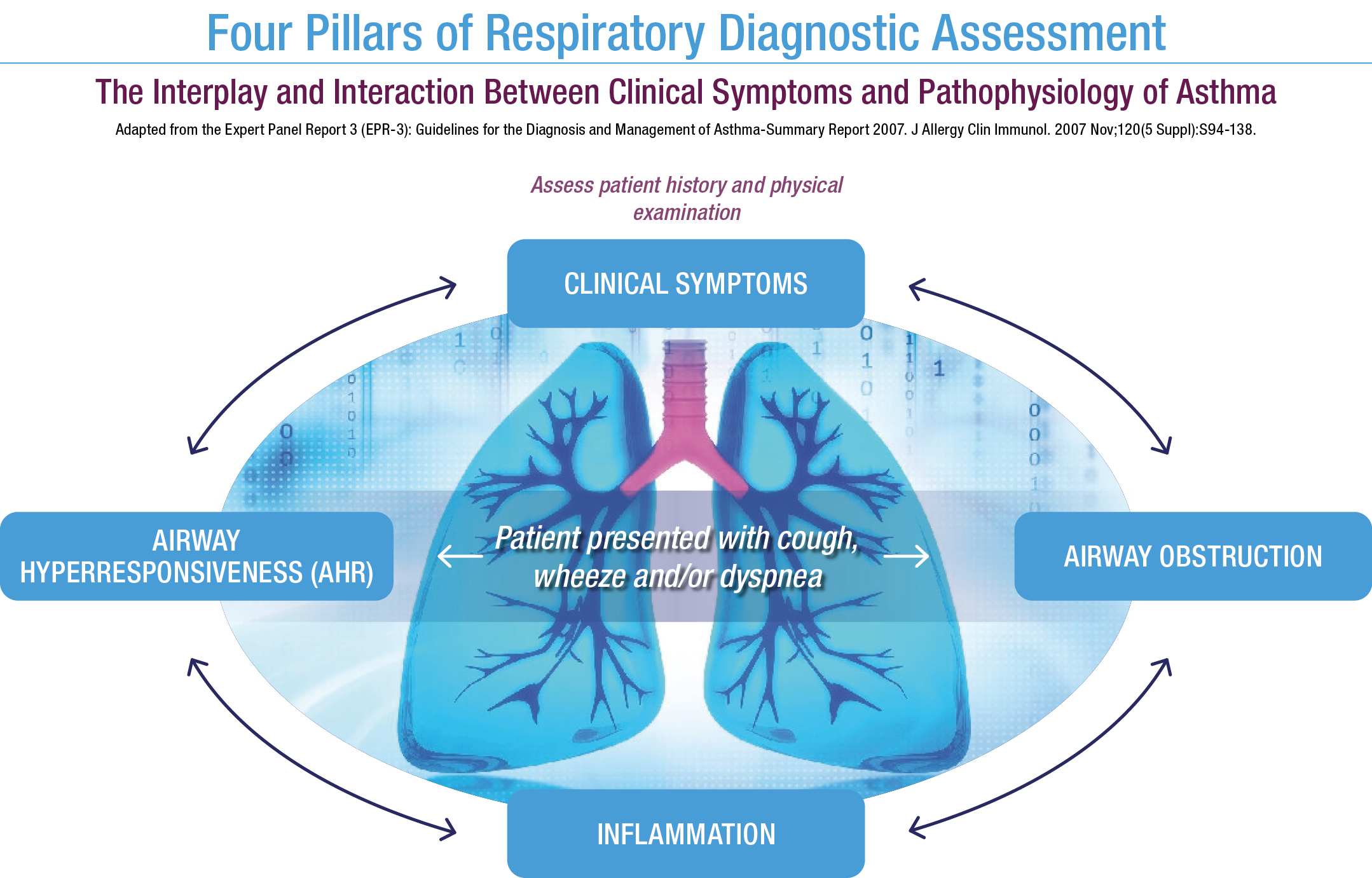
We recognize that asthma can be complex in diagnosis as well as management. Regardless of the severity of a patient’s asthma, the goal is the same, minimize symptoms and exacerbations of asthma by utilizing appropriate therapeutic intervention. There are many pieces to complete the puzzle to deliver quality patient care. By routinely assessing the four pillars of asthma, we can assist our patients in living fully. The four pillars are: clinical symptoms, airway obstruction, airway hyperresponsiveness and inflammation. Each are unique in their presentation for our patients. Recognizing the heterogeneity of asthma highlights the importance of assessing each pillar over time with every patient.
Starting with clinical symptoms. This is the key first step in the diagnostic process. Gathering a detailed history and physical is recommended. In discussing symptoms and any identified triggers, variations of the previous should also be discussed. For example. are there seasonal changes, are they at night, only during exercise, is there family history of asthma, rhinitis, etc. Often, patients can be poor historians. Incorporating questionnaires in the information gathering process is encouraged. There are many available including: The Asthma Control Test (ACT), the Childhood Asthma Control Test, the Asthma Control Questionnaire, the Asthma Therapy Assessment Questionnaire (ATAQ) control index. These are typically completed in the physician’s office prior to an appointment. If there is a need to assess on-going symptom control or therapeutic responses, a daily home diary may be employed.
While the first pillar, clinical symptoms is essential, it does not complete the patient puzzle. The second pillar, assessing airway obstruction, is important initially and with ongoing management. Utilizing Spirometry to assess obstruction is highly recommended. Patient’s perception of obstruction may be inaccurate and utilizing objective spirometry can, at times, reveal more severe obstruction than anticipated. Spirometry is recommended over peak flow measurements in the diagnostic process. Spirometry is helpful in diagnosing asthma, but it also needs to be used during patient management, particularly when there are medication changes and post-exacerbation.
As with the first pillar, the second pillar is also essential, as neither completes the entire patient puzzle. The third pillar, assessing airway hyperresponsiveness may be indicated when Spirometry is normal or near normal. Bronchial challenge tests fall in two categories, direct and indirect. Direct challenge tests, like a methacholine challenge with Provocholine®, are diagnostic for the presence of airway hyperresponsiveness (AHR), which is a characteristic feature of asthma. AHR may be seen in conditions other than asthma such as COPD or Cystic Fibrosis, so while a positive direct challenge may be consistent with asthma, the strength of the direct challenge tests is in ruling asthma out. Indirect challenge tests, such as the Aridol challenge with mannitol, can also be utilized to identify AHR. Additionally, indirect challenge tests can be used in the assessment of the fourth pillar, inflammation. The action in the airways during an indirect challenge stimulates the release of inflammatory mediators such as mast cells and eosinophils.
Inflammation is the fourth pillar in respiratory assessment. Airway inflammation needs to be monitored along with the three previously highlighted pillars. There is an interplay between the four and they are all pieces of the asthma puzzle. Inflammation can be measured through indirect challenge testing as previously stated and by noninvasively measuring FENO, fractional exhaled nitric oxide. There are other methods of assessing airway inflammation, blood work, sputum sample, bronchial biopsy and washings. FENO is a quick and easy method of measuring inflammation in the airway related to T2 inflammation. Assessing inflammation in isolation does not diagnose asthma. There are various endotypes of asthma and they do not all reflect T2 inflammation. Non T2 asthma is not eosinophilic driven and would not reflect high FENO. This stresses the importance of looking at each pillars when diagnosing and managing asthma.
How can each of the pillars contribute to asthma diagnosis?
- Clinical Symptoms If there are none, there is low probability of asthma. If clinical symptoms are reported, determine the precursors i.e. viral infection, exercise, exposure to allergen. If these are confirmed, the probability of asthma increases.
- Airway obstruction If Spirometry is normal or inconclusive, the probability of asthma is low, however it is not excluded completely if the patient has a history of clinical symptoms. If the patient shows FEV1 reversibility of ≥ 10% post bronchodilator, the likelihood of asthma is increased. If the FEV1 reversibility is ≤ 10% additional tests addressing the other pillars is indicated.
- Airway hyperresponsiveness If a direct or indirect bronchial challenge is negative, the likelihood of asthma is decreased. A positive response to a challenge test according to the parameters of the specific test performed, supports airway hyperresponsiveness as seen in asthma. Meaning the likelihood of asthma is high.
- Inflammation A positive indirect challenge confirms an inflammatory response. Measuring FENO is supportive test in diagnosis and management. FENO < 25 ppd (in adults) is normal. FENO >50 ppd indicates a high level of airway inflammation and taken with the other 3 pillars can help diagnose asthma.
What is essential to remember is that none of the pillars should be taken in isolation. All the testing recommended work together to develop the diagnosis of asthma. Each one measures, or identifies, key aspects of this complex disease. It is to our patients benefit that we understand each pillar and how they help us find the correct diagnosis and provide optimal management of asthma.
REFERENCES:
S.D. Aaron, K.L Vandemheen, et al. Reevaluation of Diagnosis in Adults with Physician-Diagnosed Asthma. JAMA. 2017 Jan 17;317(3):269-279.
Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007 Nov;120(5 Suppl):S94-138.
Dweik, P. Boggs, et al. (2011) American Thoracic Society Documents. An Official ATS Clinical Practice Guideline: Interpretation of Exhaled Nitric Oxide Levels (FENO) for Clinical Applications.
Khatri, J. Iaccarino, et al. (2021) American Thoracic Society Documents. An Official ATS Clinical Practice Guideline: Use of Fractional Exhaled Nitric Oxide to Guide the Treatment of Asthma.
Coates AL, Wanger J, Cockcroft DW, et al. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J 2017; 49. PROVOCHOLINE® package insert, revised 2/2023.
ARIDOL® package insert, revised 2/2023. 8. Porsbjerg, Celeste, et al. Current and future use of the mannitol bronchial challenge in everyday clinical practice; The clinical respiratory journal 3.4 (2009): 189-197
Author: Heather Murgatroyd, BA, RRT, CPFT
Senior Clinical Specialist